by Michael Benko
This year has been tough one for everyone including the professionals in charge of safety supplies, PPE and materials management. The struggle to keep healthcare employees safe during a pandemic is harder than it sounds. Covid-19 hit the world like a runaway train and unfortunately, it still hasn’t found its brake lever. The need for quality PPE, including isolation gowns is at an all-time high, but the supply remains elusive at best.
Prior to Covid-19, disposable isolation gowns were considered the typical answer to most Purchasing Directors’ question of “What type of isolation gown does my facility need?”. The disposable isolation gown was readily available from many overseas manufacturers, at a price that satisfied the bottom line. The number of gowns needed on any given day was low enough that any facility could order what they needed in advance and keep an ample supply level. My goodness, how things have changed.
Due to the increase in the need, and the decrease in availability, many hospitals and healthcare facilities have transitioned to reusable isolation gowns. This is not a new, or novel, idea. In fact, prior to the access to cheap plastic and polymer type materials over the last few decades, reusable items, including isolation gowns, were utilized at much higher rate than they are today. It wasn’t until the healthcare community was slapped in the face with a pandemic, and a need to change antiquated habits, that the idea and popularity of reusable isolation gowns came back into vogue. But the question that continues to come up is “Who has transitioned to, or who is already using reusable isolation gowns, and how have they done it?” The purpose of this article is to shed light on these questions.
Some proactive institutions that have led the way on this front. In some cases, due to the need that the H1N1 pandemic a few years ago revealed the lack of preparedness that the overall healthcare community was facing. In some cases, it was due to the massive amounts of waste and overuse of single use items. In other cases, it was due to the huge costs involved with having to purchase so many disposable items. Regardless of the reasons, the outcomes have been documented, and the benefits should be plastered everywhere.
Following is an excerpt from practicegreenhealth.org that was published back in December, 2015, following the impact of H1N1. The link to the article is here: https://practicegreenhealth.org/sites/default/files/upload-files/case_studies/ucla_isolation_gown_case_study.pdf
“Ronald Reagan UCLA Medical Center, located in West Los Angeles, began a reusable isolation gown pilot project in May 2012, starting with a liver transplant unit that was using 1,000 disposable isolation gowns per day. During a collaborative six-month trial period, the reusable isolation gown design was finalized and rolled out. The reusable gowns offer more comfort and better protection than their disposable counterparts, and can be laundered and reused 75-100 times. More than 3.3 million reusable gowns have been used at both hospitals since the implementation, representing a financial savings of over $1.1 million, on purchase alone. Since 2012, a total of 297 tons of waste has been diverted from landfills as a direct result of the reusable gown program.”
The savings in cost, and reduction in waste, were realized after only three years. We can only speculate the cost savings and waste reductions, since then, and since the current, arguably the worst, pandemic in modern history, Covid-19, wreaked havoc on the medical world. It goes on to say,
“Isolation gowns are used by practitioners, housekeepers, and visitors when entering the room of a patient on precaution. These gowns are single-use disposables. At Ronald Reagan UCLA Medical Center, on average approximately 6,000 gowns were being used per day (2.2 million gowns per year). In order to reduce the waste associated with isolation gowns, the academic and healthcare sides of UCLA came together in 2012 to pilot the use of reusable isolation gowns.”
It is easy to see that the benefits were plenty, and on many fronts. Although not all healthcare facilities were as forward thinking as UCLA prior to Covid-19, many have since made the transition to reusable isolation gowns since, due to the caring need that they were confronted with.
In a more recent article written by Will Maddox, published in Healthcare Business in May, 2020, and posted on dmagazine.com (https://www.dmagazine.com/healthcare-business/2020/05/the-case-for-reusable-ppe/), the following statements were made:
“Alan Bonds is the general manager of the North Texas Health Care Laundry, which is a nonprofit cooperative owned by Baylor Scott & White Health, Texas Health Resources, and Methodist Health that launders linens, scrubs, and gowns for 50 hospitals and 500 clinics in North Texas. The nonprofit employs 300 people and processes about 1 million pounds of hospital laundry a week. When the pandemic began to grow, he placed orders for more reusable gowns and scrubs to be ready for what he thought was coming.
As more hospitals move to reusable PPE to avoid shortages, there may be economic and environmental benefits, but making sure hospitals are prepared for a second wave is reason enough to plan ahead. “The supply chains worldwide were caught off guard, who knew this was going to happen?” Bonds says. “Everyone is trying to be prepared so that next time this happens we are not caught off guard.” “
The article goes on to state the following with multiple quotes from Dr. Cohen:
“As the pandemic took hold, PPE was suddenly in high demand and price gouging became an issue. Manufacturers of disposable equipment are based largely in China and India, which were dealing with their own economic and health issues. By early spring, supply lines were cut off. Suddenly, reusable PPE became the alternative protection gear. “Studies show that reusable items are better for the environment, reduce solid waste generation, energy, water use and cut greenhouse gas emissions,” writes Dr. Murray Cohen, a now retired infectious disease epidemiologist.”
“Reusable personal protective equipment, scrubs, patient gowns and other reusable healthcare garments have already proven safe and effective and more sustainable than disposable products,” writes Cohen, who notes that this equipment can be used 80 to 100 times rather than just once. “The utilization of reusable PPEs, once the industry standard, needs to be greatly expanded to prevent the types of shortages being experienced now at hospitals nationwide.”
The demand for reusable isolation gowns has grown exponentially and will continue to transform the norm, from disposable to reusable, for years to come. In a recent publication, even household names in the garment industry have begun to produce reusable isolation gowns. The following is an article regarding Hanes Brands, which is now producing reusable isolation gowns to be used by FEMA:
“The long-sleeve medical gowns are made from fabric designed to be splash resistant and can be washed and reused. They will be distributed by FEMA to hospitals nationwide and temporary treatment facilities.”https://www.businesswire.com/news/home/20200429005464/en/HanesBrands-Begins-Production-Medical-Gowns-Addition-Cloth
Green Leaf Medical Solutions, LLC was created to deliver the best-in-class, most comfortable, reusable, Level 2 Isolation gown to whoever needs it. To deliver it to them in the shortest time frame possible by utilizing a 100% American workforce and proudly claiming Made in the USA. But even reusable isolation gowns will eventually have to be discarded, and the idea of just reducing waste was not enough for Green Leaf Medical Solutions.
Thus, we created a closed loop system, that allows for the retired gowns to be returned to a repurposing facility, that will break down the used 100% polyester fabric and create new, usable polyester fabric. This is the closest thing the industry has to a zero-waste system, period.
EZ-USE Reusable Isolation Gowns allow for up to 50 washes before having to be retired. Once you have an order of them in rotation at your facility, you will always be only one laundry day away from a fresh, clean batch of isolation gowns. Compare that to the number of disposable gowns that you have to go through on a weekly, monthly, or annual basis. EZ-USE, Level 2 reusable isolation gowns give you the confidence that you will never run out of critical isolation gowns again.
Nevertheless, many facilities and healthcare organizations have NOT made the change to reusable isolation gowns. Many times, it is simply because of uncertainties, namely the cost and process of laundering.
First, what about the cost? We would be foolish to create a product that no one can afford. Yes, the cost to produce in the USA is more expensive than overseas production. Yes, the usage of premium materials has its price as well. That’s where the beauty of mathematics comes in. You can reuse the EZ-USE reusable isolation gown up to 50 times vs. a disposable isolation gown only being able to lawfully be used once. When you divide the cost per gown, by the number of uses, and add in the cost to launder, the cost per use is around $0.83 cents. The current cost of disposable isolation gowns is still elevated from pre-COVID pricing and can be as high a $4.00 per gown. Even at pre- COVID pricing for disposable isolation gowns, the EZ-USE Reusable Isolation Gown is a BARGAIN!
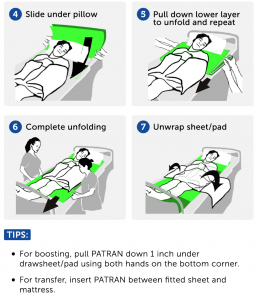
Second, the process to launder reusable isolation gowns was clearly laid out by both the CDC and Joint Commission. The process is simple, fast and the laundering process is no more arduous than washing other materials. Highlights of the procedure to launder reusable isolation gowns is as follows:
This is why so many healthcare organizations, hospitals, clinics, and even the US government have started making the transition to reusable isolation gowns. If you are on the fence about how to protect your healthcare employees, doctors, nurses, and staff, and would like to discuss how Green Leaf Medical Solutions, LLC may be able to show you that our gowns are GREENER on the other side, feel free to reach out to me anytime.
Thanks for taking the time to read. I look forward to helping you find a SOLUTION!